This week my students are looking at the non-specific immune system. As I was planning their lesson I was trying to think of what can they do that will make them think more than labelling different white blood cells? Last week, we studied antibiotics and antibiotic resistance, so I thought let’s mix the two together and have asked them to research: ‘Should we give patients with acute lymphoblastic leukaemia antibiotics before they become infected with a bacterial infection?’ That’s the question I am going to try to answer by the end of this blog.
What are antibiotics?
To understand what antibiotics are used for, it is important to understand that different microorganisms cause different illnesses and ailments. Microorganisms exist everywhere and many are not harmful, in fact we have trillions that live in our gut helping us digest our food, but some are harmful and these are called pathogens. Within pathogens, there are further categories, these being viruses (Covid-19), bacteria (E. coli), fungi (Athlete’s Foot) and protozoa (Malaria). In my experience, the things that have infected me most are viruses. I have about 3-4 common colds a year and at the moment we are very aware of the affect a virus can have. However, I am not going to talk about viruses today, I want to talk about bacteria.
Bacterial infections can be incredibly harmful, before the accidental discovery of penicillin, by Alexander Fleming in 1928, bacterial tonsillitis (Strep throat), a bad chest infection or an infected wound often resulted in death or caused the patient to become disabled. In fact, during World War I many soldiers died of infected wounds and many legs and arms were amputated to stop the spread of infection. Therefore, you can imagine the advance this made in medicine, suddenly many life-threatening diseases became treatable.
So, why do antibiotics kill bacteria? There are multiple ways that antibiotics can interfere with bacteria causing them to die. Firstly, some antibiotics affect the structure of a bacterium (Figure 1). A bacterium is surrounded by a peptidoglycan cell wall, which gives the structure needed for the bacterium to survive. Some antibiotics, such as penicillin, affect the integrity of this cell wall by stopping or interfering with the synthesis of peptidoglycan. Bacteria, like us, also have a genome, though it is not found neatly in the nucleus like our DNA, but is a made up of a circular loop of DNA. Antibiotics, such as ciprofloxatin, interfere with the copying of this DNA, so the bacterium can’t divide to make new bacteria; whilst antibiotics such as tetracycline stop the bacteria from making proteins.
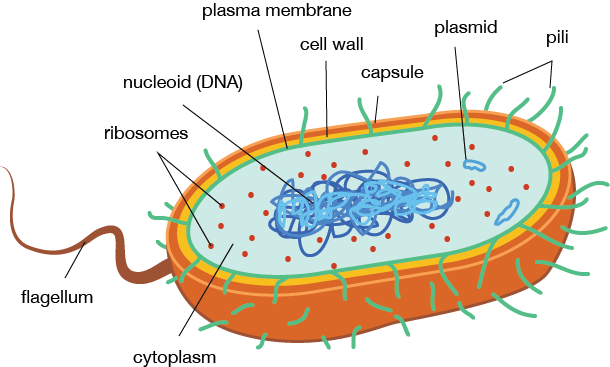
Figure 1. Structure of a Bacterium. Picture taken from [1].
With the discovery of penicillin we suddenly had the tools in our hands to be able to cure so many life-threatening diseases. Antibiotics became very widely used, in fact you could go to the doctors and ask for them just in case your cold developed into a chest infection. In some countries you could buy them over the counter, just in case. Everything bacterially was sorted, we had solved a huge problem or had we actually created an even bigger problem?
What is antibiotic resistance and where does it come from?
We thought we had conquered bacteria, but unfortunately for us, bacteria is savvier than we think. Bacteria have a trick up their sleeve, a process called bacterial conjugation. In bacterial conjugation, a donor bacterium forms a bridge between it and a recipient bacterium called a pilus. Through this pilus, the donor bacterium can pass portions of its DNA to the recipient bacterium (Figure 2). Unfortunately for us this includes sections of DNA (its genes) that code for antibiotic resistance. Once a bacteria has these genes, it means some or all of our antibiotics are useless.
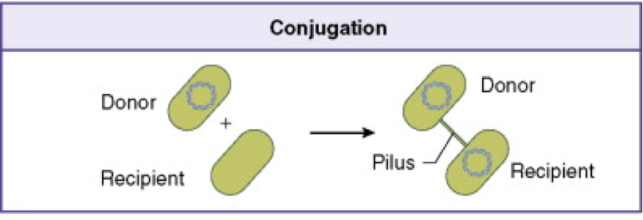
Figure 2. Bacterial Conjugation. Picture adapted from [2].
As early as 1945, Alexander Fleming was stressing that the overuse of antibiotics would lead to antibiotic resistant bacteria becoming prevalent. Antibiotics speed up the evolution of bacteria, by the process of Natural Selection. It is commonly known that in Natural Selection the strongest of the species go onto reproduce. If you are taking antibiotics you kill the ‘weakest’ in the population and leave only the ‘strong’ bacteria which are resistant to antibiotics. These strong bacteria go onto to reproduce, doubling their number every 20 minutes, until very quickly the bacteria have evolved into a new species of antibiotic resistant bacteria. This is further exacerbated by bacteria passing on their resistant genes through bacterial conjugation. Eventually, you will have an infection which can’t be treated with antibiotics. We have already seen the effects of this with infections such as MRSA causing fatalities in hospitals.
This is why your doctor will not prescribe you antibiotics when you have a cold or the flu, no matter how ill you feel. They will not work and if you do have a small underlying bacterial infection, which your body can fight easily, the antibiotics would leave you with only the resistant bacteria, making you even more poorly. Taking antibiotics when you do not need them is detrimental to your health!
It’s not just in treating ourselves that we have overused antibiotics, but in agriculture as well. Animals that are farmed, particularly intensively farmed animals, are routinely given antibiotics to prevent outbreaks of disease. However, this has lead to antibiotic resistant bacteria reproducing in farm animals. Also, the ways that animals are given antibiotics have led to increased resistance. To be able to administer antibiotics to multiple animals at once, antibiotics are often added to the water or feed that the animals eat or drink. In some cases, it has been found that these antibiotics run into the watercourse after the food or water is slopped away. If other animals, including humans, then ingest these antibiotics it furthers the evolution of antibiotic resistant bacteria.
This is a massive problem, it is estimated that worldwide 750,000 deaths are caused each year by antibiotic resistance [3]. This will only get worse as resistance starts to grow. Therefore, antibiotic resistance is a public health emergency and we need to stop the overuse of antibiotics as soon as possible.
Are there any circumstances in which you should give people antibiotics to prevent an infection?
The answer to this is yes. There are some diseases that affect the immune system, which means that a small number of vulnerable patients might benefit from receiving antibiotics as a precaution. One of these diseases is acute lymphoblastic leukaemia. Acute lymphoblastic leukaemia is a type of blood cancer which affects the white blood cells, these are the cells that destroy any pathogens that enter our bloodstream. Without these white blood cells, patients are more prone to life-threatening bacterial infections. Therefore, a doctor may decide that as a precaution, this small number of patients would benefit from the help of antibiotics. However, I am not a doctor and there will be many other factors involved in this decision including if the antibiotics will make that person ill or if they will interfere with treatment.
Take Home Message
Overuse of antibiotics has caused, is causing and will continue to cause major problems in the treatment of bacterial infections. For small groups of specific patients, they can be a good precautionary measure, but for the majority of us some Lemsip will do the trick. Therefore, as individuals we must make sure we respect antibiotics by only taking them when we really, really need them and making sure we complete the course of antibiotics given, even if they’re giving us tummy trouble, we don’t want to leave any bacteria and give them the chance to become resistant.
References
- MEDICAL-LABS, Bacteria-Cell Structure [online] 2014. Accessed on: 4th May 2020. http://www.medical-labs.net/bacteria-cell-structure-1061/
- SCIENCE DIRECT, Bacterial Conjugation [online] Elsevier, B.V 2020. Accessed on: 4th May 2020. https://www.sciencedirect.com/topics/biochemistry-genetics-and-molecular-biology/bacterial-conjugation
- REACT, The Global Threat of Antibiotic Resistance [online] Sida, Uppsala University. Accessed on: 4th May 2020. https://www.reactgroup.org/antibiotic-resistance/the-threat/